Ulcerative colitis, a chronic inflammatory bowel disease, can significantly impact the lives of those affected. In this comprehensive guide, we will delve into the complexities of ulcerative colitis, exploring its causes, symptoms, diagnosis, and effective management strategies. Understanding this condition is crucial for individuals facing its challenges, as well as for healthcare providers working towards improved patient outcomes.
Ulcerative colitis, a chronic inflammatory bowel disease, can significantly impact the lives of those affected. In this comprehensive guide, we will delve into the complexities of ulcerative colitis, exploring its causes, symptoms, diagnosis, and effective management strategies. Understanding this condition is crucial for individuals facing its challenges, as well as for healthcare providers working towards improved patient outcomes.
Unveiling Ulcerative Colitis
Defining Ulcerative Colitis
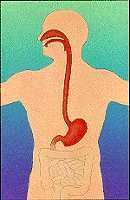
Ulcerative colitis is an inflammatory condition that primarily affects the colon and rectum. It belongs to the broader category of inflammatory bowel diseases (IBD), characterized by chronic inflammation and ulceration of the intestinal lining. Unlike Crohn's disease, which can affect any part of the digestive tract, ulcerative colitis is specific to the colon.
The Immune System's Role
The exact cause of ulcerative colitis remains unknown, but it is widely believed to involve an abnormal immune response. In individuals with ulcerative colitis, the immune system mistakenly targets the cells of the colon, triggering inflammation and the formation of ulcers.
Identifying the Symptoms
Gastrointestinal Distress
Common symptoms of ulcerative colitis include abdominal pain, cramping, and persistent diarrhea. The inflammation and ulcers in the colon can lead to an urgent need to empty the bowels, contributing to the distressing nature of the condition.
Rectal Bleeding
One hallmark symptom of ulcerative colitis is rectal bleeding. Blood in the stool or visible during bowel movements is indicative of inflammation in the rectum or lower colon. It's crucial to promptly address rectal bleeding to prevent complications.
Weight Loss and Fatigue
Chronic inflammation and diarrhea can lead to weight loss and fatigue in individuals with ulcerative colitis. Nutrient absorption may be compromised, contributing to these systemic symptoms.
Diagnosis of Ulcerative Colitis
Clinical Evaluation
Diagnosing ulcerative colitis involves a thorough clinical evaluation. Healthcare providers consider the patient's medical history, symptoms, and conduct a physical examination to assess overall health.
Endoscopy and Colonoscopy
Endoscopic procedures, such as colonoscopy, play a pivotal role in diagnosing ulcerative colitis. These procedures allow direct visualization of the colon's interior, enabling healthcare providers to identify inflammation, ulcers, and the extent of the disease.
Biopsy
During endoscopy, healthcare providers may take tissue samples (biopsies) from the colon for microscopic examination. Biopsies help confirm the diagnosis and differentiate ulcerative colitis from other gastrointestinal conditions.
Classifying Ulcerative Colitis
Categories of Ulcerative Colitis
Ulcerative colitis is categorized based on the location and severity of inflammation. Categories include ulcerative proctitis (limited to the rectum), left-sided colitis (involving the left side of the colon), and extensive colitis (affecting the entire colon).
Disease Severity
Healthcare providers often assess the severity of ulcerative colitis to guide treatment decisions. Mild cases may involve intermittent symptoms, while severe cases can lead to frequent, intense symptoms and potential complications.
Management and Treatment
Medications for Symptom Control
Various medications are used to manage symptoms and induce remission in ulcerative colitis. Anti-inflammatory drugs, immunosuppressants, and biologics are among the options, with the choice tailored to the individual's condition and response.
Lifestyle Modifications
Certain lifestyle changes can complement medical treatments for ulcerative colitis. Dietary adjustments, stress management, and regular exercise are recognized as valuable components of a comprehensive management plan.
Surgical Intervention
In cases where medications are insufficient or complications arise, surgical intervention may be considered. Surgical options range from removing the entire colon (proctocolectomy) to creating an internal pouch from the small intestine.
Living with Ulcerative Colitis
Dietary Considerations
Diet plays a significant role in managing ulcerative colitis. While specific triggers can vary among individuals, common dietary recommendations include a low-residue diet during flares and gradually reintroducing foods as symptoms improve.
Coping with Emotional Challenges
Living with a chronic condition like ulcerative colitis can be emotionally challenging. Seeking support from healthcare providers, friends, and family, as well as joining support groups, can provide valuable coping mechanisms.
Complications and Monitoring
Complications of Ulcerative Colitis
Complications of ulcerative colitis may include severe bleeding, perforation of the colon, and an increased risk of colorectal cancer, particularly in cases of long-standing inflammation.
Regular Monitoring and Follow-ups
Regular monitoring is essential for individuals with ulcerative colitis to assess disease activity, adjust treatment plans, and detect any potential complications early. Routine follow-ups with healthcare providers contribute to optimal disease management.
Emerging Therapies and Research
Advances in Medications
Ongoing research is continually uncovering new medications and therapeutic approaches for ulcerative colitis. Emerging biologics and targeted therapies offer hope for improved symptom control and long-term outcomes.
Personalized Treatment Strategies
The era of personalized medicine is influencing the management of ulcerative colitis. Tailoring treatment strategies to an individual's unique characteristics, including genetic factors, holds promise for more effective and personalized care.
Conclusion
In conclusion, ulcerative colitis is a multifaceted condition that requires a comprehensive and personalized approach to management. By understanding the causes, recognizing symptoms, and exploring effective treatment options, individuals can navigate the challenges of living with ulcerative colitis. Ongoing research, advancements in therapies, and a collaborative effort between healthcare providers and patients offer hope for improved outcomes and an enhanced quality of life.
Disclaimer:
The information on this website is provided for educational and information purposes only and is not medical advice. Always consult with a licensed medical provider and follow their recommendations regardless of what you read on this website. If you think you are having a medical emergency, dial 911 or go to the nearest emergency room. Links to other third-party websites are provided for your convenience only. If you decide to access any of the third-party websites, you do so entirely at your own risk and subject to the terms of use for those websites. Neither Arnon Lambroza, M.D., P.C., nor any contributor to this website, makes any representation, express or implied, regarding the information provided on this website or any information you may access on a third-party website using a link. Use of this website does not establish a doctor-patient relationship. If you would like to request an appointment with a health care provider, please call our office at 212-517-7570.